COPD Management: Steps That Could Improve Daily Life
Breathing well is something many take for granted until it becomes a daily challenge. Now, experts are discussing surprising ways to support lung function and energy. From overlooked breathing techniques to environment-friendly tips, these insights could make everyday life feel lighter.
Chronic Obstructive Pulmonary Disease (COPD) affects millions of Americans, causing breathing difficulties that can significantly impact daily functioning. While there is no cure for COPD, proper management strategies can help control symptoms, reduce complications, and improve overall quality of life. This article explores practical steps that individuals with COPD can incorporate into their daily routines to better manage their condition and maintain greater independence and comfort.
Why Clean Air Matters for COPD Patients
The quality of air that COPD patients breathe has a direct impact on their respiratory symptoms and overall health. Indoor air pollution can be particularly problematic, as many people spend up to 90% of their time indoors. Common indoor irritants include dust, pet dander, mold, chemical cleaning products, and smoke residue. Installing high-efficiency particulate air (HEPA) filters in home ventilation systems can remove many of these particles from the air. Regular dusting with damp cloths, vacuuming with HEPA-filtered vacuums, and controlling humidity levels between 40-50% can also significantly reduce airborne irritants. During high outdoor pollution days or pollen seasons, keeping windows closed and using air conditioning can provide additional protection.
How Light Activity Supports Lung Function
Regular physical activity might seem counterintuitive for those who experience breathlessness, but appropriate exercise actually strengthens respiratory muscles and improves oxygen utilization. Low-impact activities such as walking, gentle swimming, or stationary cycling for even 10-15 minutes daily can gradually build stamina and reduce shortness of breath over time. Pulmonary rehabilitation programs, which combine exercise training with education about COPD management, have been shown to improve exercise capacity and quality of life. These programs teach patients how to pace activities and incorporate rest periods to conserve energy while remaining active. Always consult with healthcare providers before beginning any exercise program to ensure activities are appropriate for individual capabilities.
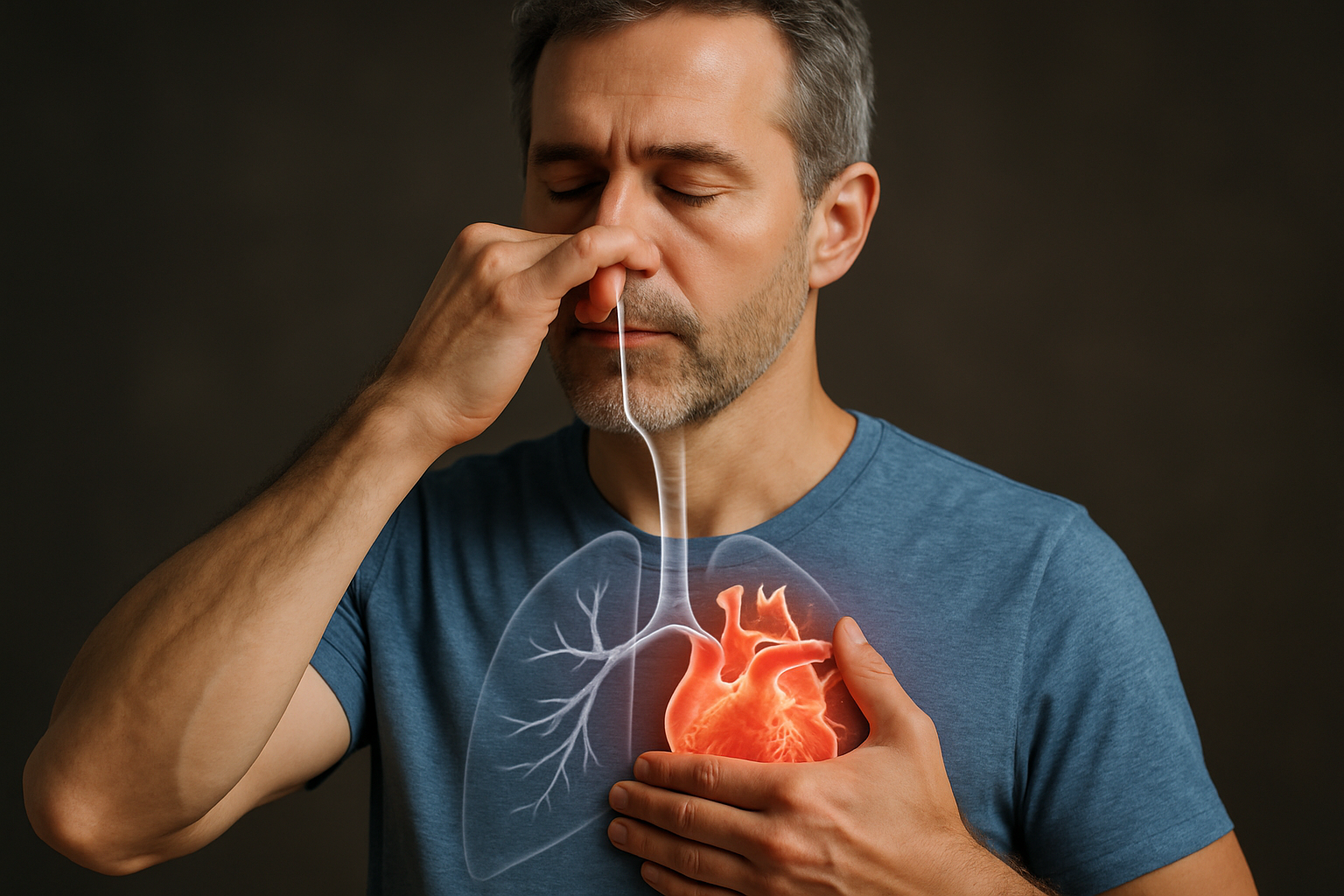
Breathing Practices That Help Manage Symptoms
Specific breathing techniques can help COPD patients manage breathlessness and improve oxygen efficiency. Pursed-lip breathing involves inhaling slowly through the nose for two counts and exhaling through pursed lips for four counts, which helps keep airways open longer and releases trapped air from the lungs. Diaphragmatic (belly) breathing strengthens the diaphragm, allowing more efficient breathing with less effort. Regular practice of these techniques, especially during periods of increased breathlessness, can provide immediate relief and long-term benefits. Some patients also benefit from devices like incentive spirometers that encourage deep breathing and help maintain lung function. Incorporating these breathing exercises into daily routines, such as during television commercial breaks or before meals, can help make them habitual.
How Nutrition Affects Energy Levels with COPD
Proper nutrition plays a crucial role in managing COPD symptoms and maintaining energy levels. Breathing difficulties require more energy, sometimes increasing caloric needs by 10 times compared to people without COPD. Consuming smaller, more frequent meals can prevent fullness that might restrict diaphragm movement and cause breathing difficulty. Foods rich in antioxidants (colorful fruits and vegetables) may help reduce inflammation in the airways. Adequate protein intake supports respiratory muscle strength, while limiting sodium can help prevent fluid retention that might complicate breathing. Some COPD patients benefit from nutritional supplements recommended by healthcare providers to address specific deficiencies. Staying well-hydrated (unless fluid restrictions have been prescribed) helps keep mucus thin and easier to clear from the airways.
The Importance of Avoiding Smoke and Other Irritants
Smoking cessation remains the single most important step for anyone with COPD who still smokes. Quitting smoking can slow disease progression and immediately improve symptoms. Even secondhand smoke exposure should be strictly avoided. Other respiratory irritants to minimize include strong perfumes, scented products, aerosol sprays, and fumes from paint, varnish, or certain cleaning products. When exposure to irritants is unavoidable, wearing a mask designed to filter particulate matter can provide some protection. Weather conditions can also act as triggers; cold, dry air can cause bronchospasm, while high humidity can feel suffocating. Planning outdoor activities according to weather forecasts and air quality reports can help minimize symptom flare-ups.
Medication Adherence and Oxygen Therapy
Consistent use of prescribed medications forms the foundation of effective COPD management. Bronchodilators help open airways, while anti-inflammatory medications reduce airway swelling. Using these medications exactly as prescribed—even when feeling well—helps prevent exacerbations. For patients prescribed supplemental oxygen, following the recommended flow rates and duration can significantly improve energy levels, sleep quality, and overall function. Modern portable oxygen concentrators allow greater mobility than traditional oxygen tanks. Some patients benefit from nebulizer treatments, which deliver medication directly to the lungs in mist form. Working closely with healthcare providers to review and adjust medication regimens as needed ensures optimal symptom control.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Conclusion
Living with COPD requires adaptations, but implementing these management strategies can significantly improve daily functioning and quality of life. Clean air environments, appropriate physical activity, effective breathing techniques, proper nutrition, and avoidance of respiratory irritants all contribute to better symptom control. When combined with proper medication adherence and regular medical follow-up, these approaches create a comprehensive management plan that helps individuals with COPD maintain greater independence and enjoy improved well-being despite their condition. The key to success lies in consistency and making these practices part of everyday life.




